In recent years, there has been increasing scientific and practical interest in extending Hippocrates’ famous saying about maximizing the therapeutic properties of food. The potential of dietary interventions should be more widely used in clinical practice. In particular, it is necessary to initiate individual dietary changes aimed at controlling normal weight, increasing adherence to healthy eating patterns, and using dietary supplements with folic acid, iodine, iron, vitamin D, and omega-3 polyunsaturated fatty acids where indicated.
Reproductive health is an extremely important target for preventive and therapeutic clinical interventions. Moreover, the current demographic situation in European countries, and especially in Ukraine, makes measures to improve the ability to have healthy offspring urgent for public health for Ukrainians of reproductive age.
In addition to changes in diet and lifestyle, modern reproductive medicine offers several innovative treatment methods that can help couples with difficulties conceiving. Among such methods is mitochondrial donation, known as the “three-parent baby” method. This technology allows replacing defective mitochondria in the mother’s egg with healthy ones from a donor, ensuring the birth of a healthy child using the genetic material of both parents. Such achievements significantly expand the possibilities for couples in fighting genetic diseases and infertility.
It is worth noting that adherence to healthy eating and lifestyle, in general, is becoming increasingly popular. However, there are still many reserves in improving eating habits and choosing healthier foods, dishes, and beverages. The possibilities of restoring fertility in men and women through dietary interventions are the subject of a growing number of studies.
Reproductive dysfunction, defined as the inability to conceive within 12 months of regular sexual activity without contraception, is common among 15-25% of married couples in Western countries. Despite the increasing use of modern reproductive technologies, the proportion of successful fertilizations has not significantly increased. Therefore, the search for additional possibilities related to lifestyle and dietary changes remains relevant.
Impact of Couple’s Age on Reproductive Function
With age, the probability of conception gradually decreases, requiring appropriate adjustments in family and career planning. Women’s fertility significantly decreases after age 35. Several studies show a 40% reduction in reproductive ability in this age group compared to women aged 20-25 years.
In older age groups, the male partner’s age has an increasing impact on a woman’s chances of getting pregnant. For example, in female age groups 19-26 years, 27-34 years, and 35-39 years, the probability of conception was 50%, 40%, and 30% respectively if the man was the same age, but decreased to 45%, 40%, and 15% if the partner was five years older.
Preconception Health and Risks
Preconception health is a woman’s health status before pregnancy. The term defines a set of indicators and risk factors that can complicate fertilization or fetal development. For example, certain foods, habits, and many pharmacological and even herbal preparations can harm the future child even before fertilization occurs.
Key preconception risks that should be identified timely with subsequent prescription of individual effective interventions to eliminate or at least reduce their impact include:
- complicated reproductive history;
- unhealthy diet, low physical activity;
- past infectious diseases, including genital infections;
- use of certain medications, dietary supplements, and herbal preparations;
- concurrent non-infectious diseases, including obesity;
- smoking, alcohol, and drug use;
- family history, presence of genetic diseases;
- psychological and social problems, psychiatric diseases.
A personalized approach with careful study of history, including reconstruction of the couple’s usual diet preferably with photo documentation of consumed dishes and beverages, critical analysis of pharmacological history, determining the appropriateness and adequacy of medication doses and dietary supplements, studying alcohol consumption levels can significantly improve control of preconception risks.
Impact of Alcohol Consumption on Reproductive Function
The consequences of alcohol consumption by women and men on fertility continue to be studied. There are understandable ethical problems with organizing randomized trials, so larger prospective cohort studies are needed to better understand the impact of alcohol (see research).
Studies examining different levels of alcohol consumption on female reproductive function show conflicting results. Moderate alcohol portions likely do not have a significant impact on fertility. At the same time, there are grounds to recommend abstaining from excessive alcohol consumption given the confirmation of several negative consequences: later pregnancies and more frequent infertility treatment consultations; impact on conception and fetal development; fetal alcohol syndrome; potentially worse results of artificial insemination.
Excessive alcohol consumption by the male partner causes deterioration of sexual gland function, including decreased testosterone production, impotence, and decreased spermatogenesis. Father’s alcohol consumption immediately before conception may be associated with heart disease in children after birth.
The level of alcohol consumption significantly affects the result of artificial insemination. The outcome worsens if both partners consume four or more portions of alcohol per week – chances of success decrease by 21% compared to those who consume up to four portions of alcohol.
Caffeine and Fertility
There is no evidence of negative effects of consuming caffeinated beverages and products on female fertility when limiting daily intake to <200 mg. There is also no data on reduced effectiveness of artificial insemination. Conversely, consuming one to five cups of coffee per day is associated with increased chances of conception. For male partners, no reproductive risks associated with coffee consumption have been established.
Impact of Insufficient Weight, Excess Weight, and Obesity on Reproductive Function
The growing popularity of strict dietary restrictions among teenage girls and young women in recent decades continues to cause great concern. One of the most dangerous forms of eating disorders shows a prevalence of 4.2% in a study conducted in Finland.
Moreover, many young girls and boys adhere to an unhealthy commitment to consuming only healthy food, known as orthorexia. It is usually associated with excluding various important food groups (meat, milk, gluten-containing grain products) and can lead to decreased body mass and deficiency of several essential nutrients.
The consequence of strict dietary restrictions combined with exhausting physical exercises can be various reproductive function disorders in women, including hypothalamic amenorrhea. Restoration of adequate caloric and balanced nutrition that ensures proper weight gain increases ovulation frequency and chances of getting pregnant.
In a study of 26 subfertile women with a body mass index (BMI) of 19.2 kg/m², all participants were offered nutritionist consultation with subsequent adherence to recommendations aimed at increasing body mass. Women gained an average of 3.7 kg, resulting in 73% of them becoming pregnant.
Excess weight and obesity are associated with disruption of all reproductive function components in women and men. Increased BMI >25.0 kg/m² (overweight) and more so >30.0 kg/m² (obesity) are associated with significant deterioration in women’s fertility.
Body mass normalization should be one of the main goals of preconception care. Results of several studies demonstrate increased probability of natural conception and reduced need for reproductive interventions due to weight loss. The latter also leads to known numerous positive consequences for overall health.
In a study including 67 women who lost an average of 10 kg over 6 months, spontaneous ovulatory cycles resumed in 60 (90%) individuals, and in 45 study participants, pregnancy resulted in childbirth.
Results of few studies indicate an association between excess weight in men and lower probability of pregnancy in their partners. In an empirical study of about 4,000 sperm donors in China, it was found that insufficient body mass (<18.5 kg/m²) is associated with lower seminal fluid concentration, decreased sperm count and motility, while with excess weight (BMI >25.0 kg/m²), decreased seminal fluid volume, sperm count, and motility were observed (see reaserach).
Impact of Adherence to Certain Dietary Models on Reproductive Function
Modern dietary patterns differ quite significantly in content of key nutrients (from macro to micronutrients), but mainly in the dominant presence of processed or natural food products.
The “Western diet,” one of the most common dietary patterns today, is characterized by consumption of large amounts of processed food high in salt, sugar, saturated fat, and simultaneously low consumption of natural plant products. Excess weight, obesity, insulin resistance, polycystic ovary syndrome, and associated reproductive function disorders have a strong association with the “Western diet.”
Optimal fertility in women and men significantly depends on constant intake of essential nutrients: proteins, quality fats, carbohydrates high in dietary fiber, vitamins, minerals, bioflavonoids, etc. Additionally, iodine, folic acid, and in some cases iron and calcium should be consumed additionally as dietary supplements.
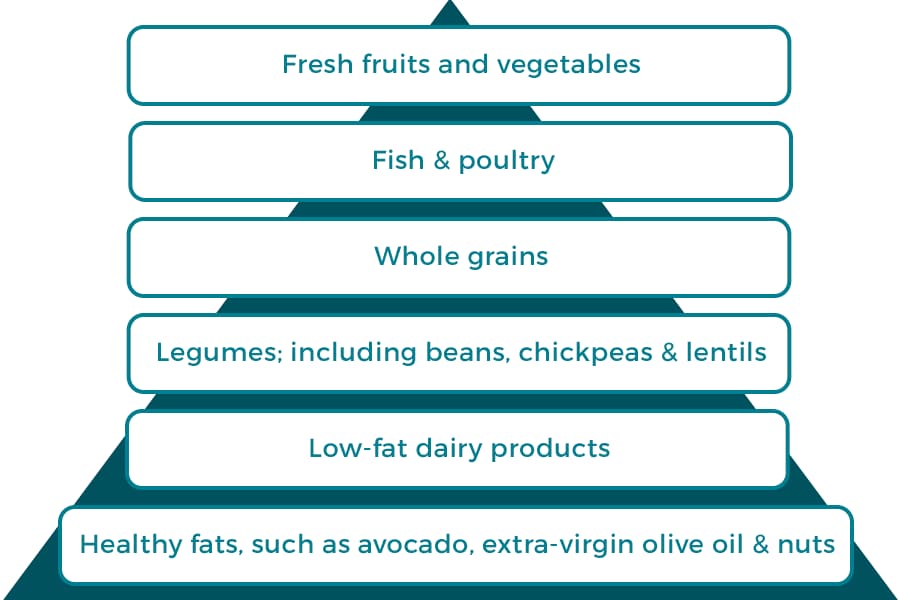
The Mediterranean diet (MD) is traditionally considered one of the best models of modern nutrition, including positive effects on fertility. In a Spanish study examining the impact of MD adherence on reproductive function, it was noted that high consumption of vegetables, fruits, whole grains and legumes, fish, poultry, olive oil (mono- and polyunsaturated fatty acids), and low-fat dairy products reduces the frequency of women’s consultations regarding conception problems by 44%.
Restrictive, Elimination Diets and Fertility
Healthy married couples, according to available reliable scientific evidence, have no proven impact on improving fertility due to following restrictive (vegetarian, low-fat, low-carb) or elimination (gluten-free, lactose-free) diets.
At the same time, undiagnosed/untreated celiac disease can lead to female and male subfertility. Reproductive function is restored through following a gluten-free diet.
“Fertile” Diet and Its Components
Conducting large-scale intervention studies to examine the impact of nutrition on fertility is methodologically complex, so dietary recommendations are based primarily on empirical research conclusions. The largest was an observation of 18,000 married women who were planning pregnancy or were already pregnant and had no history of infertility. Considering results of their own and several similar studies, the authors defined components of the “fertile” diet.
| Carbohydrates and Fats | Dairy Products and Proteins | Dietary Supplements |
| Consuming carbohydrates with a low glycemic index | Consumption of normal-fat dairy products | Use of vitamin-mineral complexes |
| High ratio of monounsaturated fatty acids to trans fats | Increased intake of plant-based proteins compared to animal-based proteins | Consumption of dietary supplements containing iron |
Healthy women whose nutrition included the above composition had significantly lower risk of ovulatory disorders. Experts consider possible favorable effects of a balanced diet on glucose metabolism and insulin sensitivity, which in turn improve ovulatory function. Other small empirical studies also indicate positive effects of MD, limiting trans fat consumption, increasing omega-3 polyunsaturated fatty acid (PUFA) content in diet for achieving natural or artificial fertilization.
In male partners, adherence to MD and other similar healthy eating patterns improves sperm quality and probability of pregnancy compared to the “Western diet.” Dietary supplements with antioxidant nutrients, including vitamins, microelements, and flavonoids, can be potentially useful additions to balanced nutrition. But the quality of evidence for their effectiveness still leaves much to be desired (see research).
Impact of Individual Food Products on Reproductive Function
Certainly, when we talk about the impact of nutrition on reproductive function realization in men and women, the primary importance rightfully belongs to the dietary pattern. Healthy, balanced diets guarantee intake of all nutrients that can promote fertility and reproductive health.
At the same time, information channels spread contradictory messages about the ability of individual food products to positively or negatively affect reproductive function. Summarized results of studies on this issue that meet evidence-based medicine standards are presented in the table.
| Food Product Group | Impact on Reproductive Function |
| Dairy and Fermented Milk Products | In the II National Health and Nutrition Examination Survey (USA), no reduction in fertility was observed with higher levels of milk consumption. |
| Meat and Processed Meat Products | The same study found that consumption of red and processed meat was associated with reduced fertility and a 1/3 increase in ovulatory dysfunction. |
| Fish and Seafood | Omega-3 PUFAs improve reproductive function. Including fatty fish (e.g., salmon, mackerel) in the diet may enhance fertility. |
| Soy Protein | Research indicates moderate consumption of soy has no significant negative impact on fertility, but excessive intake may have adverse effects due to phytoestrogens. |
| Dietary Fat | Saturated, monounsaturated, and polyunsaturated fatty acids play an essential role in maintaining reproductive function. However, trans fats significantly impair fertility, causing ovulatory dysfunction. |
It’s worth emphasizing again that adherence to a healthy, balanced diet like MD is the foundation of optimal nutrition for maintaining and restoring reproductive function. Additional strategies include higher consumption of “fertile” products and avoiding consumption of those nutrients that have negative effects, such as trans fatty acids.
Important Nutrients for Reproductive Function
Although a healthy lifestyle – including balanced and adequate caloric nutrition, regular physical activity, abstaining from smoking and alcohol consumption, sufficient sleep, and full socialization – provides conditions for maintaining fertility and fecundity, there are several nutrients whose need is increased and critically important: Iodine, Folates, Vitamin D, Iron, Omega-3 PUFAs.
Folates
Folates, also known by the alternative name vitamin B9, are extremely important for sex cells, fertilization, pregnancy development, and fetus. Natural sources of folates include green leafy vegetables, cereals, liver, and other organ meats.
The World Health Organization recommends consumption of folic acid (synthetic folate analog) at a dose of 400 mcg per day for all women of childbearing age who might become pregnant. Women who follow recommendations for folic acid intake have much lower risk of ovulation disorders and significantly shorter time to conception. It should also be noted that folic acid intake at doses >800 mcg per day significantly improves artificial insemination results.
Practical recommendations for folic acid supplementation:
- Appropriate prescription of dietary supplement “Folate 400 mcg” containing 400 mcg of metafolin – a form of folic acid with high biological activity (produced by Solgar, USA). “Folate 400 mcg” is taken as 1-2 tablets per day according to doctor’s prescriptions;
- Must also maintain a balanced diet with regular consumption of green leafy vegetables, whole grains, and liver.
Iodine
Deficiency of this microelement before conception and during pregnancy and breastfeeding causes severe irreversible consequences for child’s mental development. Pregnant and breastfeeding women’s iodine needs increase to 250-350 mcg (compared to norm for adults – 150 mcg). Given insufficient availability and low consumption of seafood naturally high in iodine, it’s recommended to use only iodized salt and additional intake of at least 100-200 mcg iodine in dietary supplements.
Practical recommendations for iodine supplementation:
- In addition to using iodized salt in food preparation, consumption of dietary supplements containing 100-200 mcg elemental iodine in daily dose is recommended;
- To ensure recommended iodine intake, vitamin-mineral complex “Multi I” (Solgar, USA) containing 150 mcg iodine per tablet can be used.
Vitamin D
Can affect reproductive function through receptors located in ovaries and endometrium. Vitamin D deficiency with significant decrease in blood levels (<20 ng/ml) is associated with risk of spontaneous pregnancy loss.
Study results indicate that women with adequate serum vitamin D levels (>30 ng/ml) have better chances of pregnancy after artificial insemination compared to those with insufficient (20-30 ng/ml) or deficient (<20 ng/ml) 25-hydroxyvitamin D levels.
Practical recommendations for ensuring optimal vitamin D levels:
- Spending 10-15 minutes per day under ultraviolet radiation in sunny weather with neck and arms uncovered;
- Consuming fatty sea fish two-three times per week;
- Consuming dietary supplements with vitamin D3 in daily dose 1200-1800 IU – 2-3 capsules per day of vitamin D3 600 IU (Solgar, USA).
Iron
Growing prevalence of iron deficiency and its clinical manifestation – iron deficiency anemia in women of reproductive age causes significant concern among specialists of various medical specialties. Control of hematological parameters and iron deficiency markers is a mandatory component of preconception care. Low serum iron levels are associated with low birth weight and increased risk of infant mortality.
Practical recommendations for preventing iron deficiency:
- Consuming sufficient food containing most bioavailable heme iron (meat, fish, organ meats);
- Simultaneous consumption of plant foods high in vitamin C, consuming tea and coffee no earlier than 1 hour after meals;
- The most effective and well-tolerated option for dietary iron supplementation is using its chelated form – iron bisglycinate. This form is found in “Gentle Iron” (Solgar, USA), taken as 1 capsule once-twice daily according to doctor’s recommendations.
Omega-3 PUFAs
Sufficient consumption of omega-3 PUFAs and their proper serum levels are associated with low risk of several dangerous diseases, including gynecological pathology that can cause subfertility. In particular, high omega-3 PUFA consumption is associated with low risk of endometriosis and higher probability of conception.
Practical recommendations for increasing omega-3 PUFA consumption:
- Consuming two-three 200g portions of fatty sea fish (primarily unsalted herring and salmon, which are the best sources of omega-3 PUFAs);
- Using dietary supplements that should provide daily amount of docosahexaenoic acid (DHA) – at least 250 mg. Recommended use of “Triple Omega-3” (Solgar, USA) as 1 capsule (378 mg DHA) once daily.
Conclusions
- Lifestyle, including dietary features, significantly affects reproductive function of men and women according to results of many studies including large cohorts in different countries.
- Daily consumption of sufficient amounts of beneficial food products according to healthy eating recommendations for adults has a significant positive impact on fertility and increases probability of conception.
- It’s worth considering the prospect of using dietary supplements with folic acid, iodine, iron, vitamin D, and omega-3 PUFAs in addition to a balanced diet, which have confirmed properties of positive impact on reproductive function.